Billing CPT 90853 sounds simple on paper. It is just “group psychotherapy,” right?
In real life, it rarely works that way.
Group therapy claims are among the most frequently denied mental health claims in the U.S.
Most practices run strong clinical programs yet lose thousands of dollars each year due to small billing mistakes. Missing documentation. Wrong diagnosis linkage. Improper session structure. Or payer rules that were never checked.
Let’s walk you through how to bill CPT 90853 correctly, step by step, from eligibility to reimbursement.
Understanding CPT 90853
Before billing correctly, you need to understand what CPT 90853 really represents.
CPT 90853 is used for group psychotherapy, in which multiple patients are treated together in a single session by a qualified provider.
The focus is on interaction, discussion, and therapeutic engagement among participants, not just education or support.
This code is not time-based. That’s important. Unlike individual therapy codes, 90853 does not require you to bill by minutes. However, that does not mean time is irrelevant. Payers still expect sessions to be clinically reasonable in length, typically 45 to 60 minutes.
Another key point. The provider must be actively facilitating therapy, not just supervising or observing.
CPT 90853 Under AMA and Medicare Guidelines
CPT 90853 is defined by the American Medical Association (AMA) under the psychotherapy section of the CPT manual. Medicare recognizes CPT 90853 as group psychotherapy when provided by an eligible behavioral health professional.
The Centers for Medicare & Medicaid Services (CMS) require that:
- The service be directed at therapeutic interaction
- Each patient receive individualized documentation
- The provider actively lead and facilitate the session
Education-only or support-only groups may not qualify as psychotherapy under Medicare rules.
Reimbursement Rates for CPT 90853
Reimbursement varies by payer and region.
On average:
- Medicare reimbursement for CPT 90853 ranges between $25 $40 per patient
- Commercial plans may pay $40 to $75 per patient, depending on contract rates
Group therapy becomes financially viable because you are reimbursed per patient rather than per session. However, improper billing can quickly wipe out that advantage.
Who Can Bill CPT 90853?
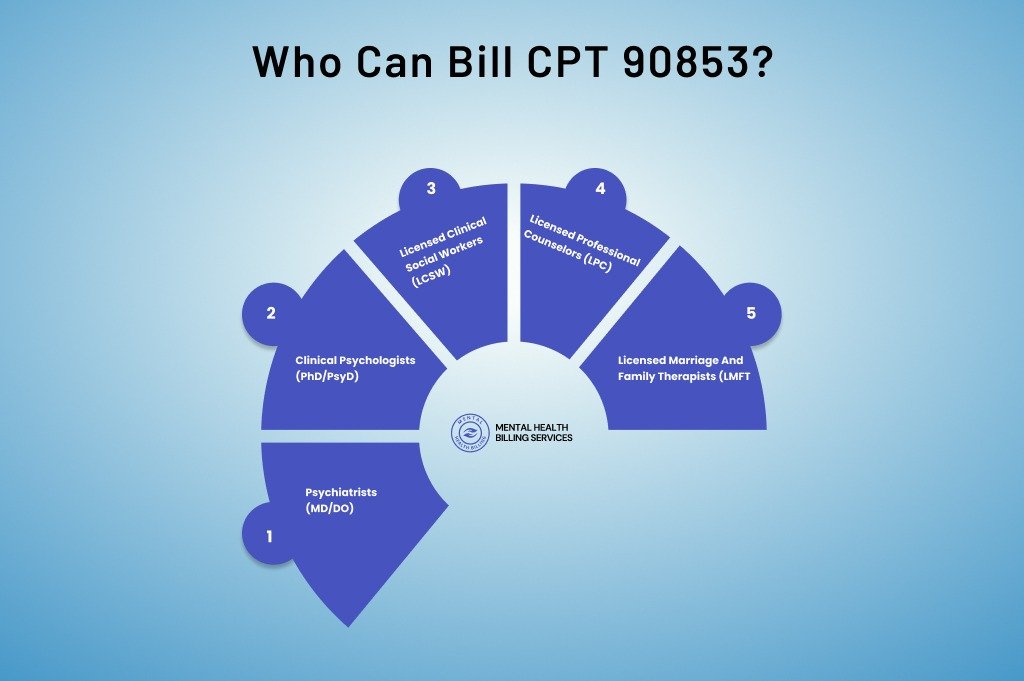
Billing eligibility depends on payer rules, provider credentials, and state regulations.
In most cases, CPT 90853 can be billed by:
- Psychiatrists (MD/DO)
- Clinical Psychologists (PhD/PsyD)
- Licensed Clinical Social Workers (LCSW)
- Licensed Professional Counselors (LPC), depending on the payer
- Licensed Marriage and Family Therapists (LMFT), depending on the payer
Medicare is stricter. It recognizes psychiatrists, psychologists, LCSWs, and certain advanced practitioners. LPCs and LMFTs are often excluded from Medicare reimbursement, though commercial plans may allow them.
Always confirm provider enrollment and credentialing before billing. I’ve seen clean claims denied simply because the rendering provider was not recognized under that plan.
Time Frame for Group Therapy Sessions
Group therapy sessions are typically structured to meet both clinical standards and payer expectations. In most cases, group sessions are conducted for a minimum of 45 minutes, which aligns with how many insurers evaluate the therapeutic value of CPT 90853. Sessions shorter than this may raise questions during claims review, primarily if documentation does not clearly support meaningful therapeutic engagement.
Group therapy is not one-size-fits-all. The actual length of each session can vary based on several factors. Insurance contract terms play a major role, as some payers outline specific expectations for session duration. The therapy modality also matters. Cognitive behavioral groups, trauma-focused groups, and substance use treatment groups may differ in structure and pacing. Frequency is another factor, since weekly groups often follow a different clinical rhythm than intensive or multiple-times-per-week programs.
When group sessions extend beyond 45 minutes, providers must pay close attention to billing rules. Some payers require the use of an add-on code when sessions exceed the standard time frame, while others consider the extended duration part of the same service. This is entirely payer-specific, which means provider manuals should be reviewed regularly before billing for longer sessions.
Session planning also impacts reimbursement. Some groups are designed to run on an open-ended basis, allowing patients to join or exit as clinically appropriate. Other groups are structured for a fixed number of weeks, such as six, eight, or twelve sessions, before formally terminating. Both models are acceptable, but insurance coverage may differ.
Many insurance companies place limits on the number of group therapy sessions they will cover within a benefit period. These limits may apply annually or per episode of care. Because of this, providers should always consider coverage limits and authorization requirements when scheduling patients into a group. Proper planning helps avoid mid-treatment denials and ensures group therapy remains both clinically effective and financially sustainable.
How to Bill CPT 90853?
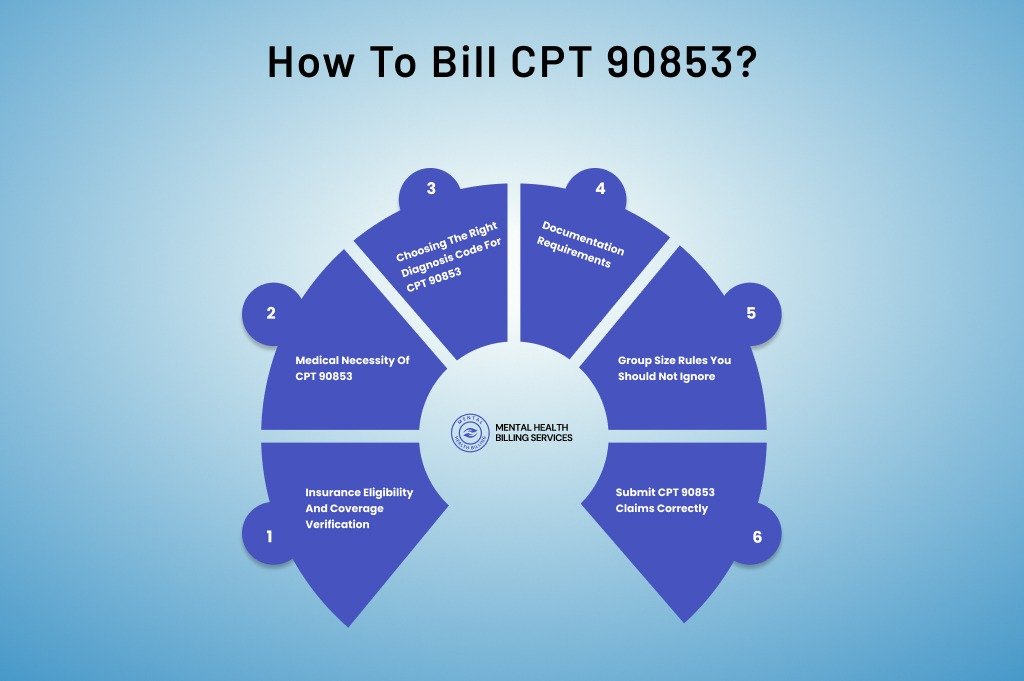
Billing CPT 90853 is not just about selecting the correct code and submitting a claim. It is a structured process that starts long before the group session begins and continues until payment is posted correctly.
From verifying coverage and confirming provider eligibility to documenting medical necessity and submitting clean claims for each patient, every step plays a role in whether reimbursement is approved or denied.
When even one part of this workflow is missed or rushed, group therapy claims quickly turn into payment delays, underpayments, or avoidable denials.
Insurance Eligibility and Coverage Verification
Before the first group session, coverage must be verified. Skipping this step leads straight to denials.
You need to confirm:
- Active mental health benefits
- Group therapy coverage under the plan
- Visit or session limits
- Copay, coinsurance, or deductible requirements
- Prior authorization rules
Some plans cover individual therapy but limit or exclude group therapy. Others cap group sessions per year.
According to industry data, over 30% of behavioral health denials stem from eligibility or authorization issues. That number alone explains why verification is not optional.
Medical Necessity of CPT 90853
No matter how clean your claim looks, it will fail without medical necessity.
Payers want to know why group therapy is appropriate for this patient.
Group therapy is typically considered medically necessary when:
- Peer interaction supports treatment goals
- The patient benefits from shared experiences
- Individual therapy alone is not sufficient
- The condition improves through group dynamics
Your documentation must explain this clearly. Not in general terms. But specifically for the patient.
A note that only describes group topics without linking them to the patient’s diagnosis and progress is weak. Weak notes get denied.
Choosing the Right Diagnosis Code for CPT 90853
Diagnosis selection is not just clinical. It is also a billing decision.
CPT 90853 must be linked to an active mental health ICD-10 diagnosis that supports psychotherapy.
Common examples include:
- Major depressive disorder (F32, F33 series)
- Anxiety disorders (F41 series)
- PTSD and trauma-related disorders (F43 series)
- Substance use disorders (F10–F19 series)
- Adjustment disorders
Avoid outdated or vague diagnoses. Make sure the diagnosis is addressed during the session and reflected in the treatment plan.
Diagnosis mismatch is one of the quietest denial triggers, especially with commercial payers.
Documentation Requirements
Many practices rely on specialized mental health billing services to review documentation before submission and prevent costly denials.
Each group therapy note should include:
- Date of service
- Session duration
- Group size
- Type of therapy used
- Provider’s active role
- Patient’s level of participation
- Progress toward treatment goals
Here is the part most providers miss.
You must document individual patient participation, even though therapy is delivered in a group.
Payers do not accept copy-paste notes across patients. Auditors look for identical language. When they find it, claims are recouped.
Each patient’s response, engagement, and progress must be clearly stated.
Group Size Rules You Should Not Ignore
There is no single national rule for group size, but payers do have expectations.
Most plans require at least two patients for CPT 90853. Typical group sizes range from four to ten participants.
Very small groups may be questioned as individual therapy. Very large groups may look more like education sessions.
If your group size falls outside the norm, document the clinical reason.
Modifiers and Place of Service for CPT 90853
CPT 90853 typically does not require time-based modifiers. However, telehealth services may require modifier 95 or GT.
Common Place of Service codes include:
- 11 (Office)
- 02 (Telehealth – not home)
- 10 (Telehealth – patient home)
Incorrect POS coding is a frequent cause of claim rejections.
Submit CPT 90853 Claims Correctly
Here is a simple but critical rule.
You bill CPT 90853 once per patient, per session.
- You do not split the code.
- You do not bill time units.
- You do not submit one claim for the entire group.
Each patient gets their own claim, tied to their diagnosis and documentation.
This is where revenue is often left on the table. Practices run whole-group sessions but underbill or bill incorrectly.
Can CPT 90853 Be Billed via Telehealth?
Yes, many payers allow CPT 90853 to be billed via telehealth, but rules vary.
Important considerations:
- Telehealth modifiers (95 or GT depending on payer)
- Correct Place of Service (POS 02 or 10)
- Platform must meet HIPAA requirements
- Group participants must be visible and actively engaged
Post-pandemic policies vary by state and payer. Always verify telebehavioral health guidelines before submitting claims.
Common Denials for CPT 90853 and How to Fix?
Denials usually fall into predictable categories.
Lack of Medical Necessity
Documentation does not clearly explain why group therapy is clinically appropriate for the individual patient. Notes focus on group discussion instead of patient progress.
How to fix it: Link the session directly to the patient’s diagnosis and treatment goals. Clearly document the patient’s participation, response, and how group interaction supports improvement.
Provider Not Eligible or Not Credentialed
The rendering provider is not recognized by the payer for group psychotherapy, especially common with Medicare and specific commercial plans.
How to fix it: Verify provider credentialing and enrollment with each payer before billing. Confirm that the provider type is eligible to bill CPT 90853 under that plan.
Service Not Covered by the Insurance Plan
Group therapy benefits were not verified, or the plan limits or excludes group sessions.
How to fix it: Verify eligibility and benefits before treatment begins. Confirm group therapy coverage, visit limits, and any required authorizations.
Incomplete or Generic Documentation
Notes are copied and pasted across patients, or lack individual participation details. Auditors flag identical or vague notes quickly.
How to fix it: Create individualized documentation for each patient. Clearly describe engagement level, therapeutic response, and progress toward goals for every session.
Incorrect Diagnosis or Diagnosis Mismatch
The diagnosis billed does not support psychotherapy or is not addressed during the session.
How to fix it: Ensure the diagnosis is active, clinically relevant, and clearly addressed in the session. Align the diagnosis with the treatment plan and progress notes.
Frequently Asked Questions About CPT 90853
Is CPT 90853 time-based?
No. CPT 90853 is not time-based, but sessions are typically 45–60 minutes.
How many patients are required for 90853?
At least two patients are required. Most groups range from 4–10 participants.
Can you bill 90853 and 90837 on the same day?
Generally no, unless separate and distinct services are documented.
Does Medicare cover group psychotherapy?
Yes, when medically necessary and provided by eligible providers.
Final Thoughts
CPT 90853 is not tricky, but it is unforgiving.
When billed correctly, group therapy can expand access to care and create stable revenue for mental health practices. When billed poorly, it becomes a denial magnet.
Focus on eligibility, documentation, and payer rules. Do that consistently, and CPT 90853 will work as intended.
Struggling With CPT 90853 Billing?
Group therapy claims are highly scrutinized, and small documentation or eligibility gaps can quickly turn into denials.
At Mental Health Billing Services, we specialize in CPT 90853 billing, documentation review, authorization management, and behavioral health revenue cycle optimization.
From Insurance eligibility verification to clean claim submission and denial resolution, our team ensures your group therapy sessions are reimbursed accurately and consistently.
If CPT 90853 claims are slowing your cash flow or increasing audit exposure, it’s time for a structured solution.
Partner with Mental Health Billing Services and turn complex group therapy billing into predictable, compliant revenue.