Behavioral health billing runs on diagnosis accuracy. No matter how strong the clinical care is, claims cannot move forward without the correct ICD-10 code. In the U.S. healthcare system, payers do not pay for services alone. They pay for medically necessary services supported by the proper diagnosis. That is where most behavioral health practices struggle.
ICD-10 codes in mental and behavioral health are detailed, layered, and closely watched. One missing digit or an outdated diagnosis can turn a clean claim into a denial.
As payers tighten utilization controls and audits increase, diagnosis-driven billing has become more critical than ever. Therapists, psychiatrists, and billing teams must work from the same playbook.
This guide explains how ICD-10 behavioral health codes work, why they matter, how payers interpret them, and how to use them across the whole billing cycle.
Understanding ICD-10 in Behavioral Health
ICD-10 stands for International Classification of Diseases, Tenth Revision. In behavioral health, most diagnosis codes fall under the F01–F99 category. These codes describe mental, emotional, and behavioral disorders.
Payers use ICD-10 codes to answer three basic questions.
- Is the condition medically necessary?
- Does it support the CPT code billed?
- Does it meet coverage guidelines for that payer?
If the answer to any one of these is no, the claim stalls.
Why Accurate ICD-10 Coding is Essential?
Behavioral health services are diagnosis-driven. Therapy time, frequency, and modality all depend on the ICD-10 code on the claim. Payers compare diagnosis severity with session length, provider type, and treatment plan.
For example, a 60-minute psychotherapy session billed with a mild adjustment disorder often raises red flags. On the other hand, major depressive disorder with recurrent episodes usually supports longer and more frequent sessions.
From a revenue standpoint, incorrect ICD-10 coding leads to:
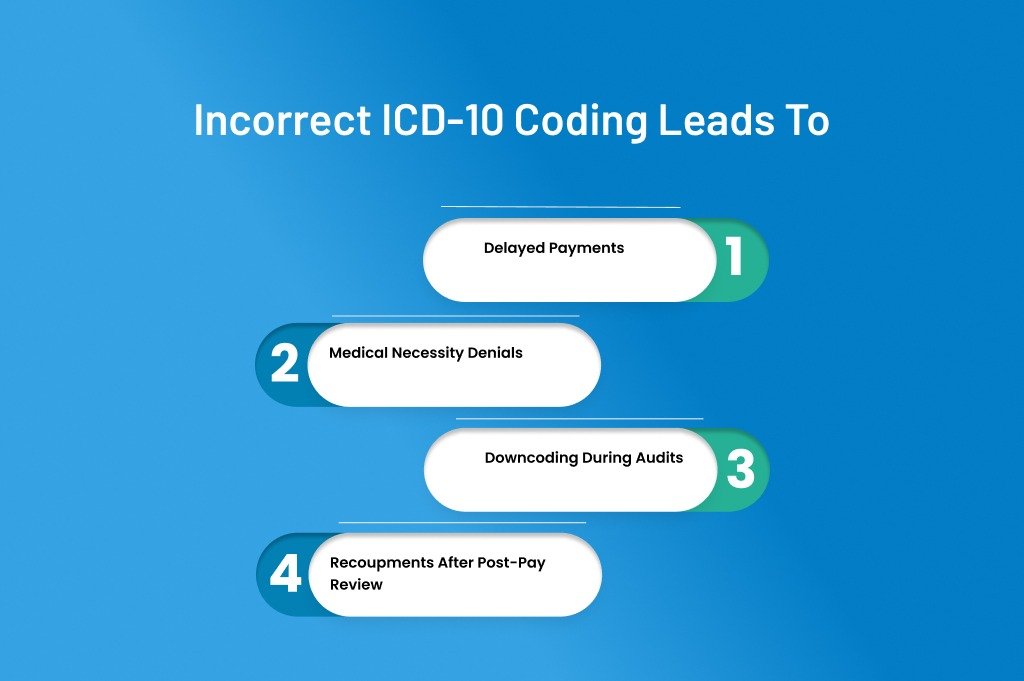
- Delayed payments
- Medical necessity denials
- Downcoding during audits
- Recoupments after post-pay review
Practices lose 5% to 10% of annual revenue due to preventable coding errors. Behavioral health is no exception.
Structure of Behavioral Health ICD-10 Codes
Behavioral health ICD-10 codes usually start with the letter F. The next two digits define the disorder group. Additional digits add detail such as severity, episode type, or remission status.
Here is how the structure works in real practice:
- F32 = Major depressive disorder, single episode
- F32.1 = Major depressive disorder, single episode, moderate
- F32.2 = Major depressive disorder, single episode, severe without psychotic features
That extra digit matters. Many payers deny unspecified codes unless documentation clearly supports them.
Common ICD-10 Code Categories in Behavioral Health
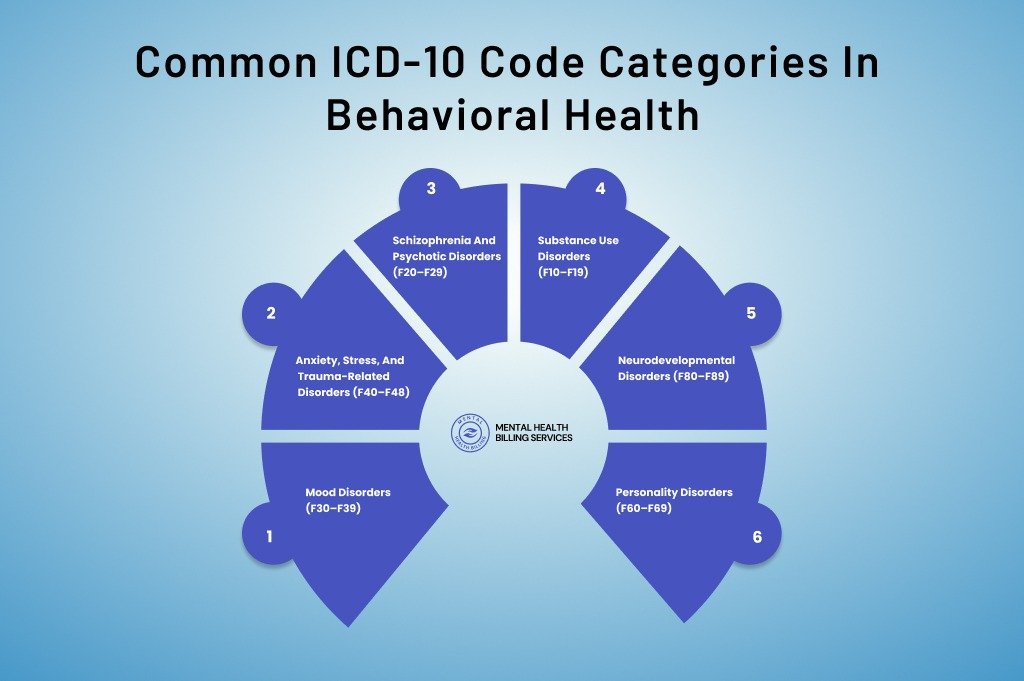
Mood Disorders (F30–F39)
Mood disorders are among the most frequently billed diagnoses in behavioral health.
Common examples include:
- Major depressive disorder (F32, F33)
- Bipolar disorder (F31)
- Persistent depressive disorder (F34.1)
Major depressive disorder alone accounts for over 25% of outpatient behavioral health claims in the U.S. Medicare and commercial payers often expect detailed severity documentation when billing psychotherapy or psychiatric management.
Avoid using unspecified depression codes when possible. Payers increasingly flag them during utilization review.
Anxiety, Stress, and Trauma-Related Disorders (F40–F48)
This category includes generalized anxiety, panic disorder, PTSD, and adjustment disorders.
Common codes include:
- F41.1 – Generalized anxiety disorder
- F43.10 – PTSD, unspecified
- F43.23 – Adjustment disorder with mixed anxiety and depressed mood
Adjustment disorders are frequently overused. While they are valid diagnoses, many payers limit long-term therapy under these codes. If symptoms persist beyond six months, documentation should justify continued treatment or support a different diagnosis.
Schizophrenia and Psychotic Disorders (F20–F29)
These diagnoses usually support higher levels of care, including frequent therapy and medication management.
Examples include:
- F20.9 – Schizophrenia, unspecified
- F25.1 – Schizoaffective disorder, depressive type
These codes often require detailed psychiatric evaluation notes. Medicare and Medicaid closely review them due to higher reimbursement and risk adjustment impact.
Substance Use Disorders (F10–F19)
Substance use coding requires special attention. ICD-10 differentiates by substance, severity, and current status.
For example:
- F10.20 – Alcohol dependence, uncomplicated
- F11.23 – Opioid dependence with withdrawal
- F12.10 – Cannabis abuse, uncomplicated
Incorrect severity selection is a common audit trigger. Documentation must clearly support abuse versus dependence. According to SAMHSA data, substance use disorder claims are audited 30% more often than standard therapy claims.
Neurodevelopmental Disorders (F80–F89)
These diagnoses are common in pediatric behavioral health and ABA services.
Examples include:
- F84.0 – Autism spectrum disorder
- F90.0 – ADHD, predominantly inattentive type
These codes usually require formal diagnostic assessments. Many payers require updated evaluations every few years to continue coverage.
Personality Disorders (F60–F69)
Personality disorders are sensitive diagnoses and must be documented carefully.
Examples include:
- F60.3 – Borderline personality disorder
- F60.2 – Antisocial personality disorder
Some commercial payers limit coverage when personality disorders are the primary diagnosis. In such cases, documenting a co-occurring condition can be critical for reimbursement.
How to Utilize ICD-10 Behavioral Health Codes in the Billing Process
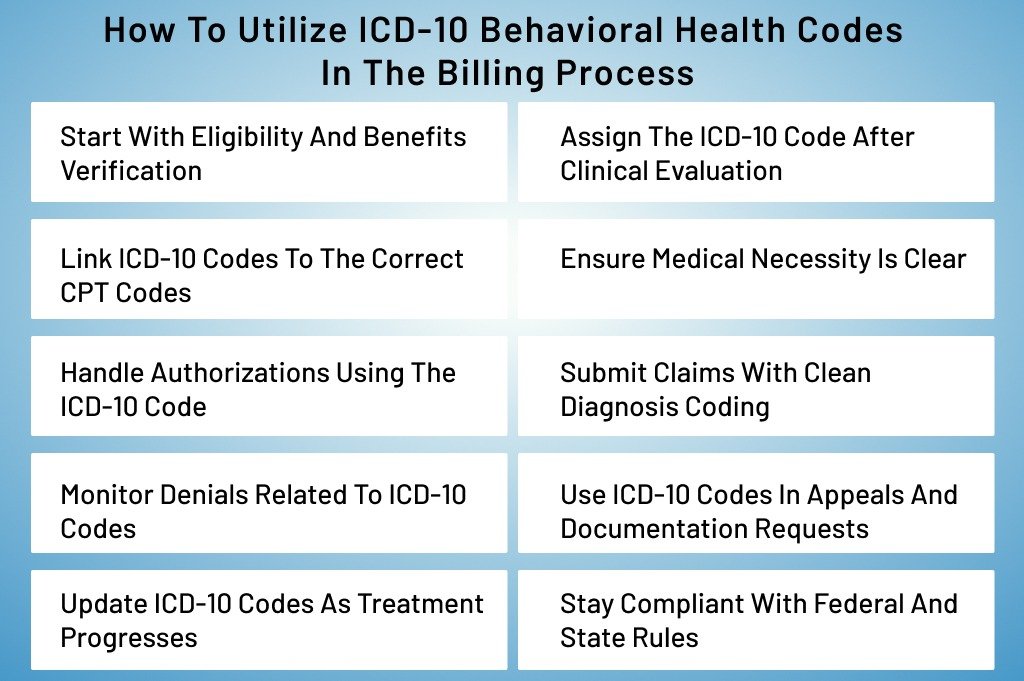
Using ICD-10 codes correctly is not just about picking a diagnosis and dropping it on a claim. In behavioral health billing, ICD-10 codes guide the entire revenue cycle. From eligibility checks to final payment posting, these codes quietly decide whether money flows smoothly or gets stuck for months.
Let’s see how to use behavioral health ICD-10 codes in the billing process for accurate billing and timely reimbursements.
Start With Eligibility and Benefits Verification
The behavioral health billing process begins before the patient ever sits down for therapy. ICD-10 codes play a role even at this early stage.
During eligibility checks, billers review whether the patient’s plan covers mental health services and which diagnoses are included or restricted. Some plans exclude certain conditions or place limits on others. For example, adjustment disorders and personality disorders are often capped or reviewed more aggressively.
Experienced billing teams use the suspected or existing diagnosis to confirm:
- Covered behavioral health conditions
- Session limits tied to specific diagnoses
- Authorization requirements
Assign the ICD-10 Code After Clinical Evaluation
The provider’s initial assessment drives the selection of ICD-10 codes. This step is clinical, but billing teams must still understand it.
The diagnosis must reflect:
- Symptoms documented
- Severity and duration
- Functional impairment
- DSM-5 alignment
In billing workflows, coders or billers review notes to confirm that the chosen ICD-10 code is specific enough. Unspecified codes may be accepted for intake visits, but they often fail for ongoing therapy.
For example, using F41.9 Anxiety disorder, unspecified, may pass once. Using it for weekly therapy over months often triggers payer review.
Link ICD-10 Codes to the Correct CPT Codes
This is where many behavioral health claims fail.
The ICD-10 diagnosis must support every CPT code billed. Payers automatically cross-check this relationship.
For instance:
- 90837 (60-minute psychotherapy) usually requires moderate to severe diagnoses
- 90791 (psychiatric diagnostic evaluation) supports a wide range of diagnoses
- Crisis codes require diagnoses showing acute distress
Billing systems flag mismatches, but payers catch what software misses. According to payer audits, diagnosis-CPT mismatch accounts for one out of every four behavioral health claim denials.
Ensure Medical Necessity Is Clear
Medical necessity is not assumed. ICD-10 codes must clearly justify why care is needed and why it continues.
Payers review:
- Diagnosis severity
- Frequency of visits
- Length of sessions
- Provider credentials
For example, weekly therapy for mild depression often gets questioned. The exact schedule for recurrent major depressive disorder is more defensible.
Billing teams work closely with providers to ensure documentation supports the ICD-10 code on file. Notes should show progress, setbacks, or continued impairment.
Handle Authorizations Using the ICD-10 Code
Many behavioral health services require prior authorization. ICD-10 codes are central to approval decisions.
When submitting authorization requests, payers look at:
- Primary diagnosis
- Secondary diagnoses
- Risk indicators
- Treatment plan goals
Incorrect or vague ICD-10 codes often lead to partial approvals or shortened authorization periods. Practices that submit detailed diagnosis information upfront experience fewer mid-treatment denials.
Submit Claims With Clean Diagnosis Coding
At claim submission, ICD-10 codes must be:
- In the correct position
- Consistent across claims
- Matched with the same CPT structure
Primary diagnosis should reflect the main reason for the visit. Secondary diagnoses should only be included if documented and relevant.
Billing systems reject claims with invalid or deleted ICD-10 codes. Payers deny claims with outdated or unsupported diagnoses.
CMS data shows that clean claims with accurate diagnosis coding are paid 30% faster than those requiring manual review.
Monitor Denials Related to ICD-10 Codes
Denials are feedback. Smart billing teams track them.
Common ICD-10 related denials include:
- Lack of medical necessity
- Diagnosis not covered
- Diagnosis inconsistent with service
- Exceeded benefit limits
When these denials repeat, it usually signals a diagnosis pattern problem, not a payer issue. Adjusting coding habits often fixes the root cause.
Use ICD-10 Codes in Appeals and Documentation Requests
When claims are denied, ICD-10 codes shape the appeal strategy.
Appeals should explain:
- Why the diagnosis supports treatment
- How symptoms impact daily function
- Why frequency and duration are appropriate
Supporting documentation must align with the ICD-10 code used. Changing diagnoses during an appeal without documentation almost always backfires.
Practices with structured appeal workflows recover 40% to 60% of denied behavioral health revenue.
Update ICD-10 Codes as Treatment Progresses
Behavioral health diagnoses evolve. Billing must evolve with them.
Symptoms may worsen, improve, or shift entirely. Keeping the same ICD-10 code for years invites audits.
Regular diagnosis reviews:
- Improve authorization renewals
- Reduce payer suspicion
- Reflect clinical reality
Medicare and many commercial payers expect diagnosis reassessment at least annually.
Stay Compliant With Federal and State Rules
Behavioral health billing is closely regulated. ICD-10 codes must comply with:
· CMS coverage policies
· State Medicaid rules
· Commercial payer medical policies
Substance use and severe mental illness diagnoses receive extra scrutiny due to funding and compliance concerns. Accurate coding protects against audits and recoupments.
Concluding Remarks
ICD-10 codes are not just clinical labels. In behavioral health, they are revenue drivers, compliance safeguards, and audit triggers all at once. When diagnosis coding is accurate, specific, and supported by documentation, claims flow. When it is rushed or outdated, revenue leaks quietly over time.
Successful behavioral health billing depends on consistency. The diagnosis must match the symptoms. The symptoms must support the CPT code. The treatment plan must justify frequency and duration. When those pieces align, payers have little reason to delay or deny payment.
As behavioral health demand continues to grow across the U.S., payer scrutiny will only increase. Automated reviews, medical necessity edits, and post-payment audits are now routine. Practices that treat ICD-10 coding as part of their revenue strategy, not an afterthought, stay ahead of those risks.
Clean diagnosis coding protects income, reduces rework, and strengthens long-term payer relationships. In behavioral health billing, getting the code right is often the difference between chasing payments and receiving them on time.