Mental health crises never follow a schedule. They show up unexpectedly, escalate fast, and demand immediate clinical attention. From a billing perspective, crisis psychotherapy is just as urgent and just as complex. CPT codes 90839 and 90840 were created to recognize this intensity. Yet these codes remain among the most misunderstood and misbilled in behavioral health.
I have seen many practices provide genuine crisis-level care but still get denied. The reason is simple. Crisis psychotherapy billing is strict. Time thresholds matter. Documentation language matters. Medical necessity matters. And payer rules vary more than most providers expect.
This guide breaks down everything you need to know about billing CPT 90839 and 90840 correctly. I will walk you through definitions, time rules, documentation, reimbursement, payer policies, denial risks, and real-world billing tips. The goal is simple. Help you get paid for the care you already provide.
What Is Crisis Psychotherapy?
Crisis psychotherapy is not just an extended therapy session. It is a distinct service designed for patients facing an immediate mental health emergency. These are moments where the patient is at high risk of harm to themselves or others, or when their psychological state has suddenly deteriorated to a dangerous level.
Think about a patient presenting with active suicidal ideation, a recent attempt, severe panic with dissociation, acute psychosis, or extreme emotional distress following trauma. In these situations, the provider is not working on long-term treatment goals. The focus is on safety, stabilization, and rapid intervention.
From a coding standpoint, crisis psychotherapy requires urgent assessment, intense therapeutic engagement, and active safety planning. Routine therapy codes do not capture this level of work. That is why CPT 90839 and 90840 exist.
CPT Code 90839
CPT 90839 represents the first 60 minutes of crisis psychotherapy provided to a patient.
This code applies when the provider delivers face-to-face psychotherapy to stabilize an acute mental health crisis. The service must involve high-intensity therapeutic intervention, not just evaluation or routine counseling.
Time is critical here. CPT 90839 covers 30 to 74 minutes of total crisis psychotherapy time on the same date of service. If the session lasts less than 30 minutes, this code cannot be billed.
The provider must be actively engaged in crisis intervention throughout the time. Passive monitoring or non-therapeutic activity does not count.
CPT Code 90840
CPT 90840 is an add-on code used when crisis psychotherapy extends beyond the first hour.
Each unit of 90840 represents an additional 30 minutes of crisis psychotherapy beyond the initial 60 minutes. This code is always billed in conjunction with 90839 and never on its own.
There is no explicit maximum number of 90840 units in the CPT manual. However, payers often apply medical necessity and reasonableness limits. Prolonged crisis sessions must be clearly justified in documentation.
Difference Between CPT 90839 and CPT 90840
Before jumping into the billing steps, it is essential to understand how these two codes work together but represent different parts of the same service.
CPT 90839 covers the initial crisis psychotherapy service, while CPT 90840 covers additional time beyond the first hour. One cannot exist without the other. 90839 is the foundation. 90840 builds on it.
Most billing errors happen when practices treat these codes like standard therapy add-ons. They are not. Crisis psychotherapy has its own rules, time thresholds, and documentation expectations.
Reimbursement Rates for CPT 90839 and 90840
Understanding reimbursement helps providers recognize when claims are underpaid or misprocessed.
While rates vary by geographic region and contract, typical reimbursement ranges include:
- Medicare reimbursement for CPT 90839: Approximately $140–$170
- Medicare reimbursement for CPT 90840: Approximately $65–$90 per additional 30-minute unit
- Commercial payer reimbursement: Often ranges between $180–$300+ depending on contract terms and provider credentials
Crisis psychotherapy generally reimburses at a higher rate than standard 60-minute therapy (CPT 90837) because it reflects increased clinical intensity and immediate risk management.
Practices should always compare paid amounts to contracted fee schedules. Underpayments frequently occur when add-on code 90840 is processed incorrectly or when time thresholds are misapplied.
Time Rules for 90839 and 90840
Time-based billing is one of the most common denial triggers for crisis psychotherapy. You must meet the minimum time requirements exactly.
For CPT 90839, the total face-to-face time must fall between 30 and 74 minutes. Once the session reaches 75 minutes, you may bill 90839 plus one unit of 90840.
Here is how time typically breaks down in practice:
A 45-minute crisis session qualifies for 90839.
A 70-minute crisis session still qualifies only for 90839.
A 90-minute crisis session qualifies for 90839 plus one unit of 90840.
A 120-minute crisis session qualifies for 90839 plus two units of 90840.
Crisis Psychotherapy Time-to-Code Breakdown
| Total Face-to-Face Time | Code(s) to Bill |
|---|---|
| 30–74 minutes | 90839 |
| 75–104 minutes | 90839 + 90840 (1 unit) |
| 105–134 minutes | 90839 + 90840 (2 units) |
| 135–164 minutes | 90839 + 90840 (3 units) |
Always document start and end times clearly. Estimated or rounded time entries increase audit risk.
What Qualifies as a Mental Health Crisis?
Not every distressed patient qualifies for crisis psychotherapy. Payers look closely at whether the situation meets the definition of a true crisis.
A qualifying crisis typically includes imminent risk, such as suicidal or homicidal ideation, severe self-harm behavior, acute psychosis, or inability to maintain safety without immediate intervention.
Emotional distress alone is not enough. Anxiety, depression, grief, or relationship conflict may feel urgent, but they do not automatically qualify unless they escalate to a safety-threatening level.
Your documentation must clearly explain why the situation required immediate crisis intervention rather than a scheduled therapy session.
When NOT to Bill CPT 90839
Not every urgent or emotionally intense session qualifies as crisis psychotherapy. Billing CPT 90839 incorrectly increases denial and audit risk.
Do not use CPT 90839 for:
- Routine therapy sessions extended due to discussion
- Mild or moderate anxiety without safety risk
- Scheduled appointments addressing chronic depression
- Medication management without active crisis intervention
- Administrative or coordination-only encounters
If the patient is distressed but not at imminent risk, standard psychotherapy codes such as 90834 or 90837 may be more appropriate.
Clear differentiation between routine therapy and crisis care strengthens compliance and protects revenue.
Who Can Bill 90839 and 90840?
Crisis psychotherapy may be billed by qualified mental health professionals acting within their scope of practice. This commonly includes psychiatrists, clinical psychologists, licensed clinical social workers, licensed professional counselors, and other credentialed behavioral health providers.
Credentialing matters. If the provider is not credentialed with the payer for psychotherapy services, claims will be denied regardless of the quality of documentation.
Supervision rules also apply. Services provided by interns or trainees must follow payer-specific supervision and billing guidelines.
Telehealth Billing for CPT 90839 and 90840
Many payers allow crisis psychotherapy to be delivered via telehealth, but billing requirements vary.
When billing crisis psychotherapy via telehealth:
- Use Modifier 95 or GT depending on payer rules
- Select the correct Place of Service (POS 02 or POS 10)
- Ensure the platform meets HIPAA compliance standards
- Document that the crisis intervention occurred in real time
Post-pandemic telebehavioral health policies continue to evolve. Always verify payer-specific telehealth coverage before claim submission.
Incorrect modifier or POS usage is a leading cause of reduced reimbursement for crisis services.
Documentation Requirements for Crisis Psychotherapy
Documentation is the backbone of successful crisis billing. Even a single missing element can trigger a denial or an audit.
Your clinical note must clearly establish that a crisis existed. Start by describing the presenting problem in urgent terms. Explain what made the situation unsafe or unstable at that moment.
Next, document the interventions used. Crisis psychotherapy involves active therapeutic techniques such as de-escalation, safety planning, risk assessment, coping strategy development, and coordination of emergency resources when needed.
Time documentation must be precise. Include start and end times and total minutes spent in crisis psychotherapy. Avoid vague phrases like “extended session.”
Finally, document the outcome. Describe how the patient’s condition changed by the end of the session and what follow-up steps were arranged.
How to Bill CPT Code 90839?
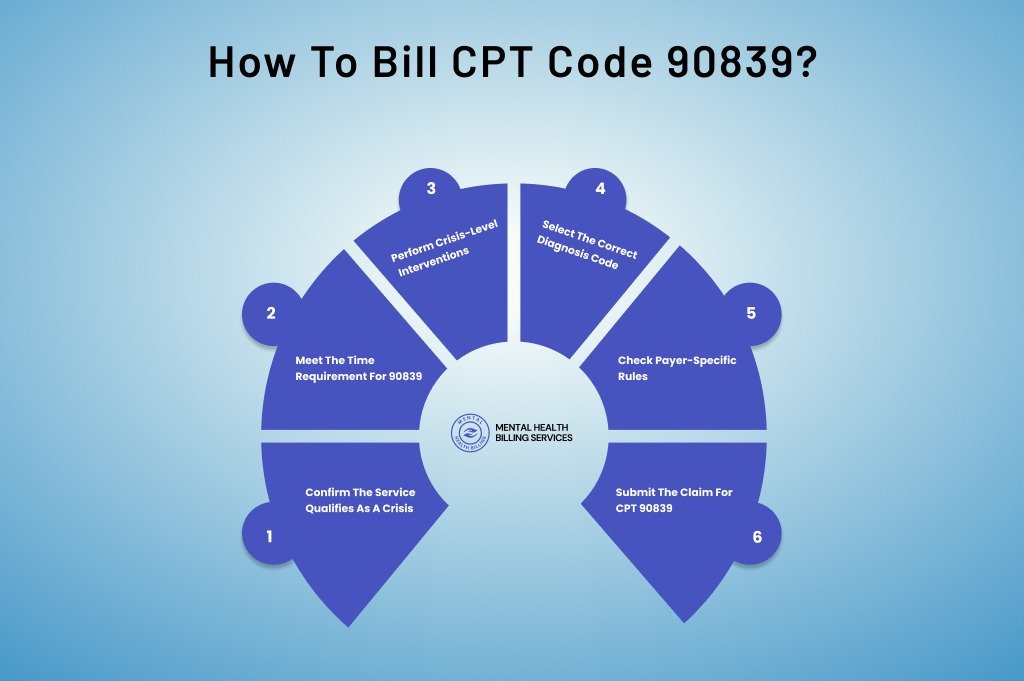
CPT 90839 represents the first 60 minutes of crisis psychotherapy, but billing starts much earlier than claim submission. It begins the moment the patient presents in crisis.
Step 1: Confirm the Service Qualifies as a Crisis
The first billing checkpoint is clinical, not administrative. The patient must be in an acute mental health crisis. This means immediate risk of harm, severe emotional instability, or a sudden psychological breakdown that cannot wait for routine therapy.
Situations like active suicidal ideation, homicidal thoughts, acute psychosis, or severe panic with loss of control usually qualify. Routine anxiety, scheduled therapy, or emotional distress without safety risk does not.
If the situation does not meet crisis criteria, CPT 90839 should not be used, no matter how long the session lasts.
Step 2: Meet the Time Requirement for 90839
Time drives this code. CPT 90839 requires 30 to 74 minutes of face-to-face crisis psychotherapy on the same date of service.
Anything under 30 minutes is not billable as 90839. Anything over 74 minutes may qualify for CPT 90840, but only after 90839 is billed.
From a billing standpoint, always document:
- Session start time
- Session end time
- Total minutes spent in crisis psychotherapy
Payers routinely deny claims when time is estimated or vaguely described.
Step 3: Perform Crisis-Level Interventions
The services provided must match the intensity of the code. Crisis psychotherapy involves active intervention, not passive listening.
Common crisis interventions include safety planning, suicide risk assessment, emotional stabilization, grounding techniques, and coordination of emergency resources when needed. Documentation should clearly reflect this intensity.
If the note reads like a standard therapy session, payers will downcode or deny the claim.
Step 4: Select the Correct Diagnosis Code
Diagnosis selection must support the crisis. Use diagnoses that reflect acute severity, not stable or mild conditions.
For example, major depressive disorder with suicidal ideation supports crisis care far better than unspecified depression. Diagnosis mismatch is a leading cause of 90839 denials across all payer types.
Step 5: Check Payer-Specific Rules
Medicare, Medicaid, and commercial payers all recognize CPT 90839, but rules vary.
Some payers restrict same-day billing with E/M services. Others require specific modifiers or place-of-service rules, especially for telehealth. Eligibility and benefits verification should always be completed before billing.
Step 6: Submit the Claim for CPT 90839
Once documentation is complete and coding is accurate, submit CPT 90839 on the claim with:
- Correct diagnosis pointer
- Correct place of service
- Appropriate modifiers if required
This completes the billing cycle for CPT 90839.
How to Bill CPT Code 90840: Complete Billing Process
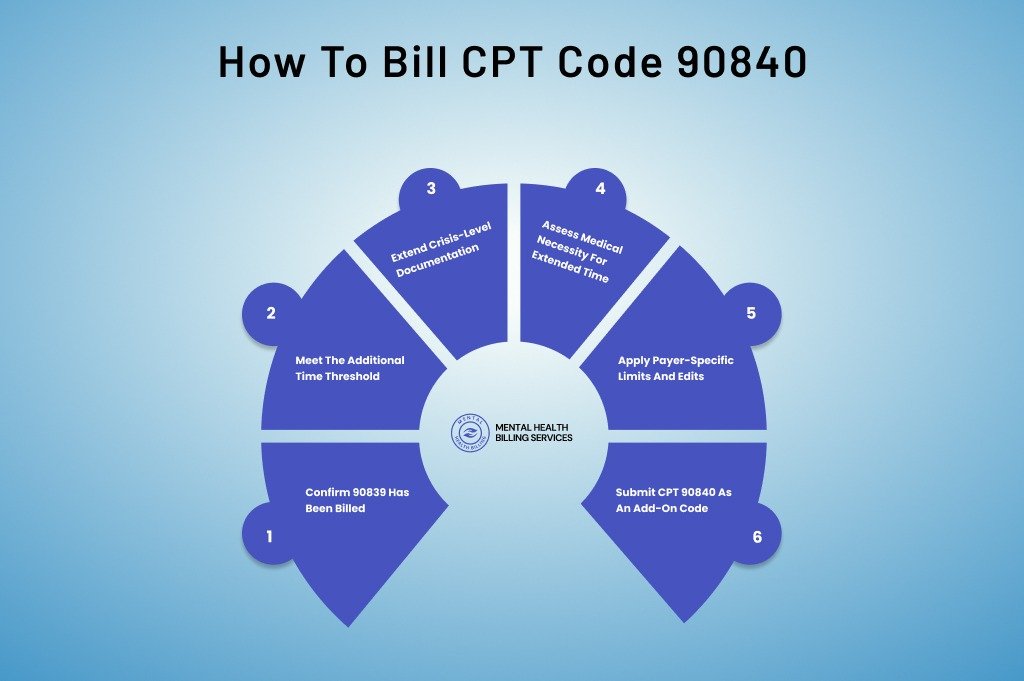
CPT 90840 is often misunderstood. It is not an independent code. It is an add-on code used only when crisis psychotherapy extends beyond the first hour.
Step 1: Confirm 90839 Has Been Billed
CPT 90840 cannot be billed alone. It must always be reported with CPT 90839 on the same date of service.
If 90839 is missing, 90840 will automatically deny, regardless of documentation quality.
Step 2: Meet the Additional Time Threshold
Each unit of CPT 90840 represents an additional 30 minutes of crisis psychotherapy beyond the initial 60 minutes.
Billing typically follows this pattern:
- 75 to 104 minutes total time allows one unit of 90840
- 105 to 134 minutes allows two units
Time must be continuous and face-to-face. Breaks or unrelated activities cannot be counted.
Step 3: Extend Crisis-Level Documentation
Documentation for CPT 90840 must show why the crisis required extended care. Payers expect to see escalating risk, difficulty stabilizing the patient, or complex safety planning.
Simply stating “session continued” is not enough. The note should explain why the crisis could not be resolved within the first hour.
Step 4: Assess Medical Necessity for Extended Time
This is where many claims fail. Payers scrutinize long crisis sessions closely. The medical necessity for the extended time must be clear.
If the patient remained actively suicidal, psychotic, or emotionally unstable, document it clearly. If progress was made slowly due to complexity, explain why.
Step 5: Apply Payer-Specific Limits and Edits
Some payers apply soft caps on the number of 90840 units billed in one day. While CPT does not list a maximum, payers may flag unusually long sessions for review.
Internal billing teams should monitor frequency and duration trends to reduce audit risk.
Step 6: Submit CPT 90840 as an Add-On Code
When submitting the claim:
- List CPT 90839 first
- Add CPT 90840 with the correct number of units
- Ensure diagnosis and place of service match the primary code
Best Practices for Providers Billing CPT 90839 and 90840
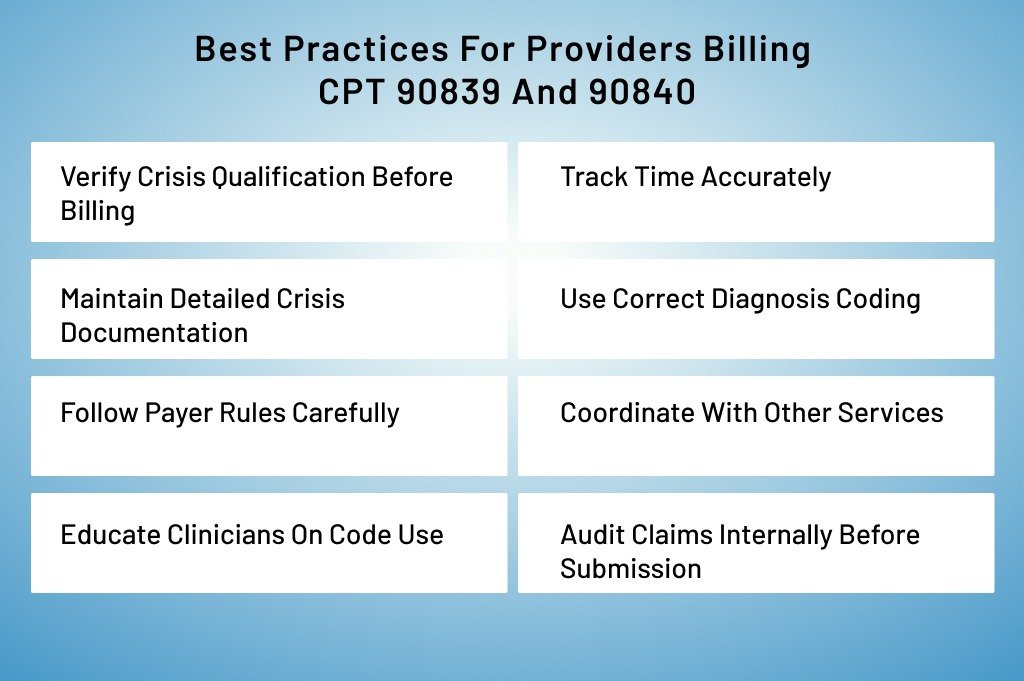
Crisis psychotherapy is high-stakes work. Patients are often at immediate risk, and clinicians must act quickly to stabilize them. From a billing standpoint, CPT 90839 and 90840 are lucrative but also highly scrutinized by payers. Implementing best practices ensures providers are reimbursed correctly while maintaining compliance.
Verify Crisis Qualification Before Billing
Not every urgent or distressing session qualifies as crisis psychotherapy. Providers should confirm:
- The patient is at imminent risk of harming themselves or others.
- Symptoms are acute and severe, not chronic or stable.
- The situation requires immediate clinical intervention, not a routine therapy session.
Pro Tip: Develop a checklist for clinicians to assess whether a session meets crisis criteria quickly. This reduces errors and strengthens documentation.
Track Time Accurately
Time is the backbone of CPT 90839 and 90840. Providers should:
- Document start and end times for each session.
- Record total face-to-face minutes clearly in the progress note.
- Track additional 30-minute increments for 90840 when sessions exceed 60 minutes.
Pro Tip: Many EMR systems allow auto-time stamps. Using these reduces estimation errors and helps defend claims in audits.
Maintain Detailed Crisis Documentation
Documentation must prove both the existence of a crisis and the clinical interventions provided. Include:
- A clear description of the crisis and why immediate intervention was necessary.
- Therapeutic interventions used, such as de-escalation, safety planning, grounding techniques, or coordination with emergency services.
- Patient response and outcome at the end of the session.
- Any follow-up plans or next steps.
Pro Tip: Use structured templates in the EMR specifically for crisis psychotherapy. This ensures that all required elements are consistently included.
Use Correct Diagnosis Coding
Selecting a diagnosis that reflects acute risk or severity is critical. Providers should:
- Avoid vague or mild diagnoses for crisis sessions.
- Align the diagnosis with documented symptoms and risk.
- For suicidal or homicidal ideation, use the appropriate ICD-10 codes that reflect acute severity (e.g., F32.2 Major depressive disorder, single episode, severe without psychotic features).
Pro Tip: Train clinicians on diagnosis selection to minimize denials. Pair this with internal auditing to catch mismatches early.
Follow Payer Rules Carefully
Most payers recognize crisis psychotherapy, but rules differ:
- Medicare: Reimburses CPT 90839 and 90840 but may limit telehealth use and same-day billing with E/M.
- Commercial payers: Often scrutinize extended sessions, require modifiers, or have preauthorization policies.
- Medicaid: State-specific regulations apply. Some allow telehealth; others require in-person sessions.
Pro Tip: Maintain a payer reference sheet with documentation, time, and telehealth requirements for crisis codes. Update it regularly.
Coordinate with Other Services
Crisis psychotherapy may occur alongside other interventions:
- E/M services: Bill separately with modifier 25 if services are distinct.
- Inpatient or ED care: Coordinate with facility billing to avoid duplication.
Pro Tip: Always note when the crisis session overlaps with other treatments. Clear differentiation in the documentation prevents denials.
Educate Clinicians on Code Use
Misuse often stems from a lack of understanding. Providers should know:
- CPT 90839 is for the first 60 minutes of crisis psychotherapy.
- CPT 90840 is an add-on time after 60 minutes.
- Both codes require documentation that proves intensity, time, and medical necessity.
Pro Tip: Host quarterly training sessions or create quick-reference guides for crisis codes. Include examples of properly documented sessions.
Audit Claims Internally Before Submission
Regular audits catch errors before claims reach payers. Check for:
- Time documentation errors
- Missing or insufficient crisis detail
- Diagnosis mismatch
- Correct use of CPT 90840 as an add-on
Pro Tip: Flag high-risk claims for secondary review. This is especially important for extended sessions lasting more than 90 minutes.
Frequently Asked Questions About CPT 90839 and 90840
What is the minimum time required for CPT 90839?
A minimum of 30 minutes of face-to-face crisis psychotherapy is required.
Can CPT 90839 and 99213 be billed on the same day?
Yes, if the evaluation and management service is separate and distinct from the crisis psychotherapy. Modifier 25 may be required.
Is CPT 90839 covered by Medicare?
Yes, when medically necessary and provided by an eligible behavioral health professional.
Can CPT 90840 be billed alone?
No. CPT 90840 is an add-on code and must always be billed with 90839.
Does crisis psychotherapy require preauthorization?
Some commercial payers may require authorization depending on the patient’s plan. Always verify benefits prior to billing.
Final Thoughts
Crisis psychotherapy is demanding work. It requires clinical skill, emotional presence, and rapid decision-making. CPT codes 90839 and 90840 exist to recognize that intensity, but they demand accuracy in return.
When billed correctly, these codes support fair reimbursement and reflect the actual value of crisis care. When billed incorrectly, they invite denials and audits.
By understanding time rules, documentation standards, and payer expectations, you can protect your revenue while continuing to provide critical care when patients need it most.
Struggling With Crisis Psychotherapy Billing?
CPT 90839 and 90840 are high-value codes, but small documentation or time errors can trigger costly denials.
Our mental health billing services include crisis claim review, documentation audits, telehealth compliance checks, and structured revenue cycle management for behavioral health providers.
If crisis claims are being reduced, denied, or audited, now is the time to protect your reimbursement.
Schedule a Behavioral Health Billing Review and ensure your crisis services are paid accurately and consistently.